Nasr City, 52 El Tayaran Street, in front of the Health Insurance Hospital

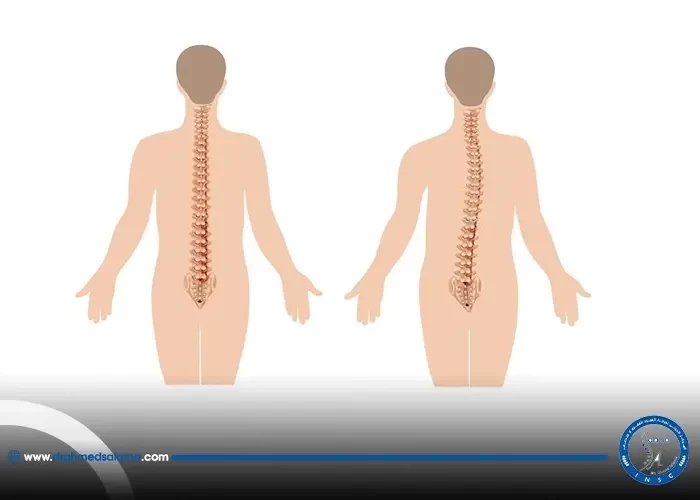
Pregnancy after spinal fusion surgery

For many women, cervical surgery is a necessary procedure to treat certain medical conditions. However, it can also raise concerns when it comes to pregnancy. There are several factors to consider when planning a pregnancy after cervical surgery, such as the type of surgery performed and the timing of conception. In this blog post, we will explore the topic of pregnancy after cervical surgery and provide valuable information for women who are planning to conceive.
Introduction: The Need for Pregnancy Management Following Cervical Surgery
After undergoing cervical surgery, it is necessary to manage a subsequent pregnancy with care in order to ensure a healthy outcome for both the mother and baby. Cervical laser surgery, as well as other ablative and excisional procedures, can have an impact on the ability to conceive and carry a pregnancy to term. Complications and risk factors may arise during pregnancy if adequate management is not put in place. It is important to consider recovery time, sexual activity, and trying to conceive after surgery to avoid unforeseen complications. While early-stage cervical cancer treatment and fertility-sparing surgery options are available, a radical hysterectomy may limit the possibility for future pregnancies. Therefore, it is crucial to consider any treatment option in relation to future pregnancy plans in order to make an informed decision. Overall, pregnancy management following cervical surgery is essential for a safe and healthy pregnancy journey.
Cervical Laser Surgery: Effect on Pregnancy and Conception
In the second section of the blog, the focus is on the effects of cervical laser surgery on pregnancy and conception. The good news is that this type of surgery appears to have no negative impact on a woman's ability to conceive or carry a pregnancy to term. Furthermore, other treatments for abnormal cervical cells, such as cold coagulation, cryotherapy, and laser therapy, are also unlikely to affect fertility. Though some treatments can lead to a small increase in the risk of preterm delivery or cervical incompetence, overall, it is safe to try to conceive after cervical surgery. Of course, individual factors and case-specific concerns should always be discussed with a qualified healthcare provider.
Pregnancy Complications and Risk Factors After Cervical Surgery
After cervical surgery, there is an amplified risk of adverse pregnancy outcomes such as preterm birth, low birth weight, and pregnancy loss. Pregnant patients with advanced cervical dysplasia or a history of surgical excision should be considered high-risk pregnancies. Some women may need surgery to stretch (dilate) the cervix to prevent complications during pregnancy. However, studies have shown that no miscarriages, stillbirths, or severe obstetric complications occurred until delivery. It is important to disclose any past pregnancy complications or surgeries to the healthcare provider for proper management during and after pregnancy. Furthermore, cervical trauma may result from some surgical procedures used to treat cervical abnormalities associated with an abnormal Pap smear. It is crucial to consider the potential risks and complications before proceeding with cervical surgery for women who plan to conceive in the future.
Statistics: Pregnancy Loss After Ablative and Excisional Surgery
The risk of pregnancy loss after cervical surgery is a concern for many women who have undergone ablative or excisional treatment for cervical intraepithelial neoplasia. According to statistics, 21 percent of women who underwent cervical surgery experienced pregnancy loss, with rates slightly higher for those who underwent ablative treatment. However, it's important to note that the risk of pregnancy loss is still relatively low, with only a small percentage of women experiencing this outcome. It's also important to consider individual factors that may increase the risk of pregnancy loss, such as age or other medical conditions. Women who have undergone cervical surgery should discuss their individual risk with their healthcare provider and work together to develop a plan for monitoring their pregnancy and managing any potential complications.
Recovery Time and Sexual Activity After Cervical Surgery
After cervical surgery, it is important to allow your body time to recover before resuming sexual activity. Recovery time depends on the type of surgery performed, but generally, it takes about 4 to 6 weeks for the cervix to heal. It is important to follow the recommendations of your physician and avoid any activities that could disrupt the healing process. This may include abstaining from sexual activity, using tampons, or douching. It is normal to experience some bleeding after treatment for abnormal cervical cells, but your doctor will advise you on how long to avoid certain activities. It is important to maintain open communication with your physician and carefully consider the timing of sexual activity when planning for pregnancy after cervical surgery.
Trying to Conceive After LEEP: Timeframe and Healing Duration
After a LEEP procedure, it can take up to six months for the cervix to fully heal. During this time, it's recommended that women avoid sex or inserting anything into the vagina for four weeks. Trying to conceive too soon after the procedure can increase the risk of complications during pregnancy, such as premature birth or miscarriage. To avoid these risks, patients are usually recommended to wait six months before trying to conceive on their own. If pregnancy does not occur within this timeframe, further fertility treatments may be considered. It's important to consider the healing duration and timeframes for pregnancy after cervical surgery to ensure safe and healthy outcomes.
Treatment Options for Early-Stage Cervical Cancer and Fertility
Treatment options for early-stage cervical cancer, such as radical hysterectomy and trachelectomy, can have significant implications on fertility. While radical hysterectomy remains the gold standard, trachelectomy may offer a reasonable fertility-sparing option for eligible patients. However, the decision to undergo either surgery should also consider individual factors such as cancer stage, age, and desired future pregnancy. Women who have undergone cervical surgery may still be able to conceive and carry a healthy pregnancy, but may require specialized pregnancy management and monitoring. It is important for these patients to discuss their fertility options and potential risks with their healthcare providers to make informed decisions regarding their cancer treatment and future family planning.
Pregnancy After Radical Hysterectomy: Possibilities and Limitations
After undergoing a radical hysterectomy, becoming pregnant is no longer possible as the uterus and cervix have been removed. This major surgery may present limitations and complications for women who desire to have children in the future. However, alternative options such as adoption or surrogacy can still be pursued. It is important for women to discuss their fertility options and desires with their healthcare provider before undergoing hysterectomy. Additionally, finding emotional support and resources can be helpful in navigating the emotions that may arise following this life-altering surgery. Despite the limitations of radical hysterectomy, the procedure has proven to have high success rates in treating early-stage cervical cancer and improving overall health outcomes for women.
Success Rates of Surgery for Cervical Cancer and Pregnancy Outcomes
Section 9 explores the success rates of surgery for cervical cancer and its impact on pregnancy outcomes. While cervical cancer surgery is often associated with complications and risks for pregnancy, studies have shown that fertility-sparing surgery, such as radical trachelectomy or cone biopsy, can lead to successful pregnancies. In fact, one study showed a live birth rate of 73.3% for women with early-stage cervical cancer who underwent fertility-sparing surgery. However, it's important to note that pregnancy after cervical surgery can still come with potential complications, such as preterm delivery and miscarriage. Patients should discuss their options and risks with their healthcare provider to make an informed decision about their fertility and pregnancy planning after cervical surgery.
Conclusion: Considerations for Cervical Surgery and Pregnancy Planning
In conclusion, considering the potential impact of cervical surgery on pregnancy and fertility is crucial for women who have undergone such procedures. Prenatal care management, including cervical cerclage, may be necessary to prevent preterm birth and other pregnancy complications. It is reassuring to note that there is no evidence suggesting that cervical intraepithelial neoplasia treatment negatively affects fertility. However, patients should discuss their fertility concerns with their healthcare provider before undergoing cervical surgery. It is also imperative to follow postoperative instructions and allow for adequate healing time before attempting to conceive. With careful planning and monitoring, women can have successful pregnancies after cervical surgery.
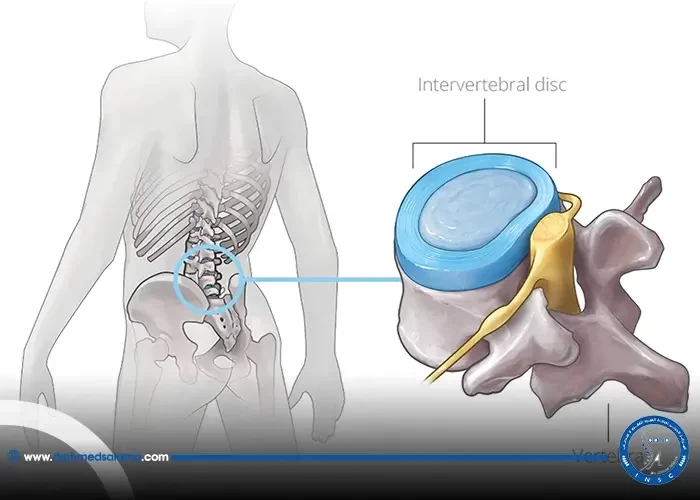
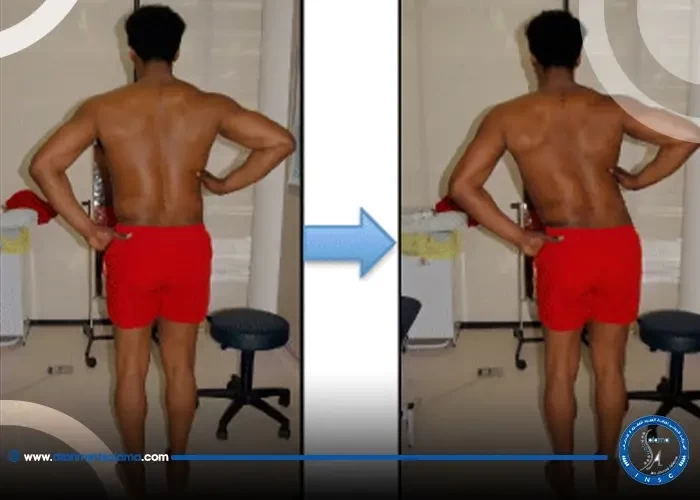
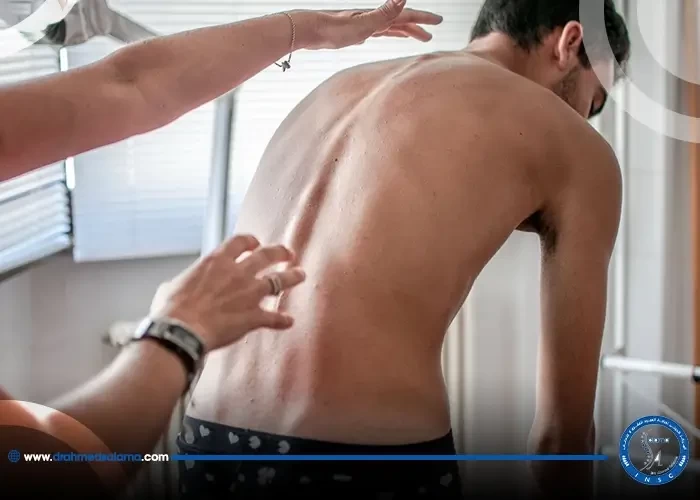
Is it possible to get pregnant after a spinal fusion surgery?
Yes, absolutely, a woman can become pregnant, give birth, and breastfeed naturally after a spinal fusion surgery, provided that the vertebrae have fully healed.
What is the success rate of vertebral fusion surgery?
The success rate for spinal fusion surgery ranges from 70 to 90%. The more skilled the doctor, the more prepared the center, and the more committed the patient is to instructions, the higher the success rate.