Nasr City, 52 El Tayaran Street, in front of the Health Insurance Hospital

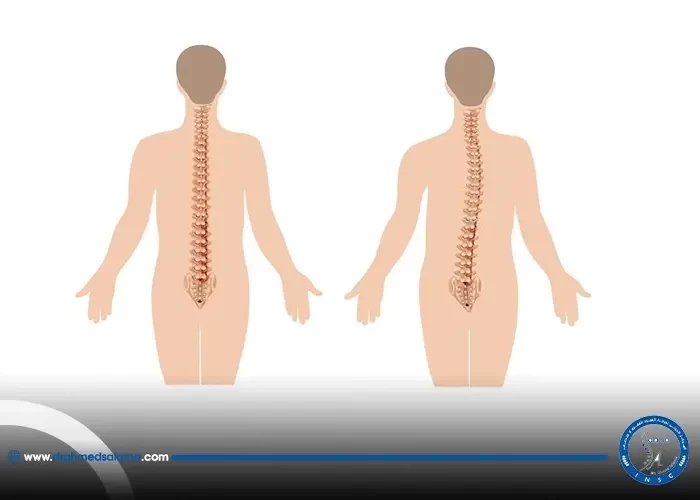
Cartilage removal and stabilization of vertebrae
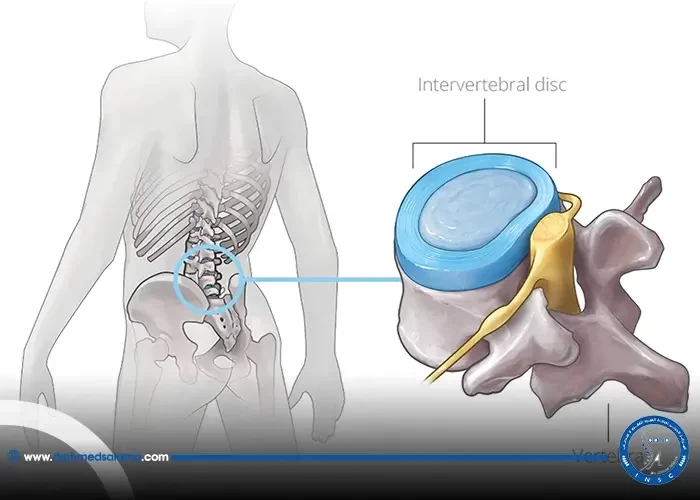
Cartilage removal and vertebrae fixation are two common medical procedures used to relieve back pain and spinal conditions. Cartilage removal can help alleviate joint pain caused by wear and tear, while vertebrae fixation can stabilize a spinal column that is prone to shifting. Both procedures are generally safe and effective, but require precision and expertise from skilled medical professionals. In this blog post, we will explore the ins and outs of cartilage removal and vertebrae fixation in plain English, providing readers with a better understanding of these important medical interventions.
Introduction to cartilage removal and vertebrae fixation
In the world of orthopedic surgery, procedures involving cartilage removal and vertebrae fixation are commonplace. These surgeries aim to repair damage and stimulate new cartilage growth, as well as reduce pressure on the spinal cord and nerves. Techniques such as internal fixation with screws and wire, bone fusion surgery, and neural canal expansion with plates and screws are often used. Imaging tests are used to determine when to consider surgery, and doctors use various types of decompression techniques for spinal disc issues. Such surgeries are also performed for knee meniscus injuries and glenoid labral injuries. These procedures require a complex and dynamic interface between surgical implants and bodily tissue, and proper care must be taken to prevent complications.
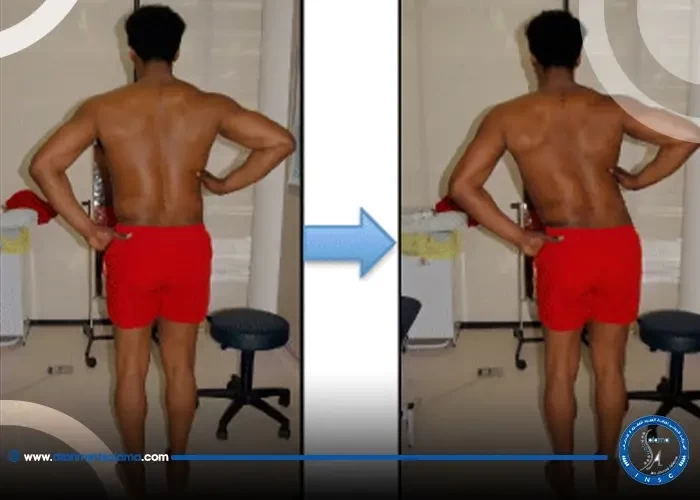
Internal fixation of the spine without fusion
Internal fixation of the spine without fusion is a non-fusion method used in the treatment of thoracolumbar fractures, spondylolisthesis, and other spinal conditions. In this technique, screws, rods, and plates are used to stabilize the spine without actually fusing it. This technique allows for faster recovery times and preserves the natural mobility of the spine. However, internal fixation may not be suitable for all patients and cases. Depending on the severity of the spinal condition, fusion may be necessary. It is important to consult with a spine specialist to determine the best treatment plan for each individual case.
Spinal cartilage surgery for herniated discs and tumors
Spinal cartilage surgery is a common procedure used to treat herniated discs or tumors that cause pain and discomfort. This surgical technique involves removing or repairing the damaged cartilage in the spine in order to alleviate pressure on the affected area. In conjunction with other spinal fixation techniques, such as screws and wire, this surgery can provide a long-term solution for patients suffering from debilitating spinal conditions. It is critical to work closely with a qualified healthcare provider to determine the best course of treatment for your individual needs. Other sections of this blog also outline different types of spinal fixation methods and imaging tests used by doctors to diagnose spinal issues. Ultimately, understanding the various options available to you and working closely with your doctor can help you achieve optimal spinal health and quality of life.
Spinal fixation with screws and wire
Spinal fixation with screws and wire is a commonly used method for stabilizing vertebrae that have been damaged or improperly aligned. This internal fixation technique involves attaching small metal screws and wires to adjacent vertebrae in order to hold them in place while they heal or fuse together. In some cases, this approach can be used as an alternative to bone fusion surgery. This section of the blog builds on the previous sections discussing spinal cartilage surgery, bone fusion surgery in the neck, and neural canal expansion. It highlights the importance of spinal imaging in allowing doctors to determine when and how to use these techniques, and the role of surgery in addressing spinal disc issues and herniated discs. By presenting this information in a friendly and easily understandable tone, the blog aims to provide useful context and guidance for individuals considering or undergoing spinal fixation procedures.
Bone fusion surgery in the neck
Bone fusion surgery in the neck is a common surgical procedure used to correct problems with the vertebrae in the cervical spine. This involves connecting two or more bones in the spine with metal implants, which hold the vertebrae in place until the bones fuse together. Although bone fusion surgery in the neck may help ease neck or back pain, it is a complex procedure that requires skilled surgeons and careful postoperative care. It is often used in conjunction with other spinal surgeries, including spinal cartilage surgery for herniated discs and tumors and spinal fixation with screws and wires. Patients considering bone fusion surgery in the neck should discuss their options with their doctors and undergo imaging tests to determine the best course of treatment.
Glenoid labral injuries and surgical fixation or debridement
When it comes to injuries to the glenoid labrum, surgical options include fixation or debridement, depending on the extent and location of the injury. Surgical fixation involves re-attaching the torn labrum to the bone using specially-designed suture anchors to ensure a secure approximation. On the other hand, debridement involves the removal of damaged portions of the fibrocartilage. As with all surgeries, recovery times may differ between individuals, but it is common to be on crutches for a few weeks after the surgery. Labral injuries are not uncommon and can cause significant shoulder pain. Early detection and treatment can prevent the injury from getting worse and causing further damage. It is always best to consult with a medical professional to determine the best course of action for your specific case.
Knee meniscal surgery and cartilage removal
Knee meniscal surgery and cartilage removal is a common procedure to remove or repair torn meniscus and damaged cartilage in the knee. The removal of the meniscus can lead to a decrease in knee lubrication, which can cause further damage and ultimately lead to arthritis. This is why doctors often opt for partial meniscectomies or meniscal repairs instead, in order to preserve as much of the meniscus as possible. When looking at other surgical procedures for joint health, such as spinal cartilage surgery or bone fusion surgery, it's clear that there are multiple methods for fixing joints and bones within the body, each with their own benefits and drawbacks. Ultimately, the decision to undergo surgery should come after discussing all options with a trusted medical professional and weighing the benefits and risks.
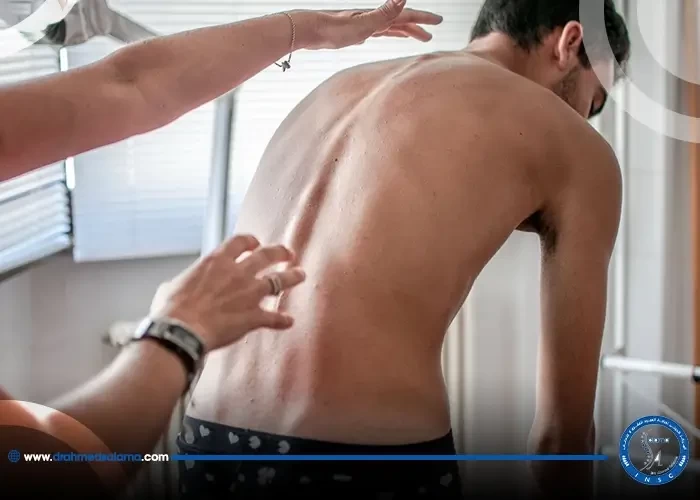
Decompression for spinal disc issues
The process of decompression is an important part of dealing with spinal disc issues. In fact, it's often the primary rationale for any form of disc prolapse surgery, where the goal is to relieve the affected nerve root and mitigate the patient's symptoms. There are different ways to approach decompression, depending on the specific location and cause of the problem. Some methods involve removing tissue such as discs, bones, or cartilage, while others focus on expanding the neural canal or performing laminectomy. The blog has also covered internal fixation techniques using screws and wire, as well as bone fusion surgery in the neck. By familiarizing themselves with these options, patients can work with their doctors to determine the best course of action for their particular situation.
Neural canal expansion and spinal fixation with plates and screws
Neural canal expansion and spinal fixation with plates and screws are methods used to treat spinal issues. This type of surgery involves creating more space within the spinal canal to alleviate pressure and compression on the nerves. The procedure can also include the insertion of metal plates and screws to stabilize the spine. This blog section builds on previous sections that discussed spinal cartilage surgery, bone fusion surgery, and internal fixation of the spine. Doctors may consider neural canal expansion and spinal fixation with plates and screws for individuals with conditions such as herniated discs or spinal stenosis. Imaging tests may be used to determine the best approach for each patient. It is important to note that surgery is not always the first option and doctors will typically explore non-surgical options before recommending this type of procedure.
When to consider spine surgery and imaging tests used by doctors
When it comes to spine surgery, it's not a decision that should be taken lightly. It's usually recommended only when the source of the pain can be pinpointed and non-surgical treatments have been exhausted. This is where imaging tests come in to play. X-rays, CT scans, and MRIs can all be used to help diagnose the problem and determine if surgery is necessary. Of course, this decision is made on an individual case-by-case basis with input from the patient's doctor. It's important to note that not everyone is a candidate for spine surgery. Factors such as joint disease, nerve compression, previous surgeries, and weight can all play a role in the decision-making process. Before considering any surgical procedure, patients should have a thorough discussion with their doctor and understand the risks and benefits involved.
Are there any complications of discectomy and vertebral fusion surgery?
Complications of discectomy and vertebral fixation rarely occur, especially when the endoscope is used to complete this procedure. The most common of these complications are swelling and redness around the wound area.
How long is the recovery period after a discectomy and vertebral fusion?
The recovery period varies from one case to another, but in general, it ranges between 6 to 12 months until the bones and vertebrae heal together.
What is the success rate of discectomy and vertebral fusion surgery?
The success rate is usually estimated between 60 and 80%, but there are some factors that affect the success rate, including the techniques used, the doctor's competence, and the extent to which the doctor's advice is followed.