Nasr City, 52 El Tayaran Street, in front of the Health Insurance Hospital

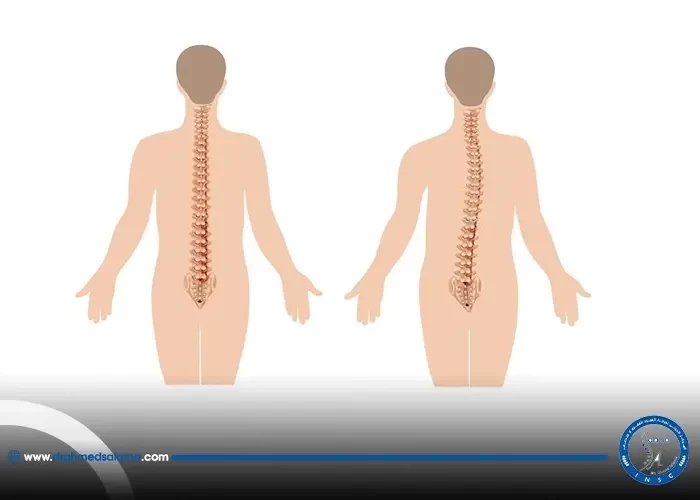
Endoscopic lumbar fusion surgery
Welcome to our blog where we explore the world of minimally invasive spine (MIS) surgery. MIS surgery is a revolutionary approach that has transformed the field of spinal surgery. This technique offers patients a safer, faster, and less painful option for treating back and neck pain compared to traditional open surgery. In this blog, we will dive into the benefits and the impact of minimally invasive spine surgery, how it is performed, and who is a candidate for the procedure. Stay tuned for valuable insights on this fascinating subject matter!
What is minimally invasive spine (MIS) surgery?
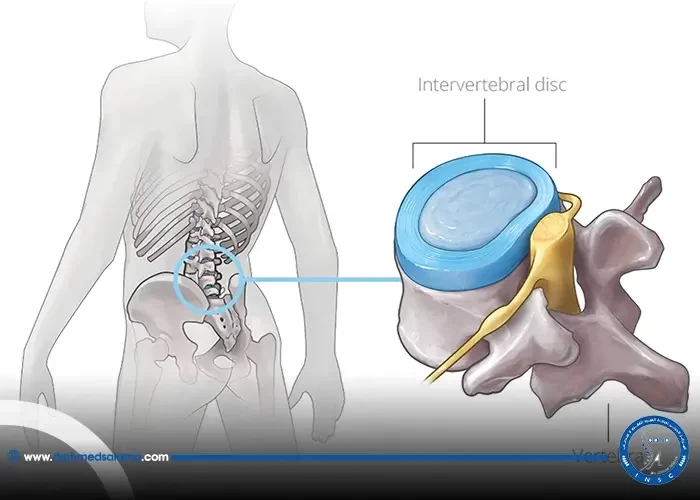
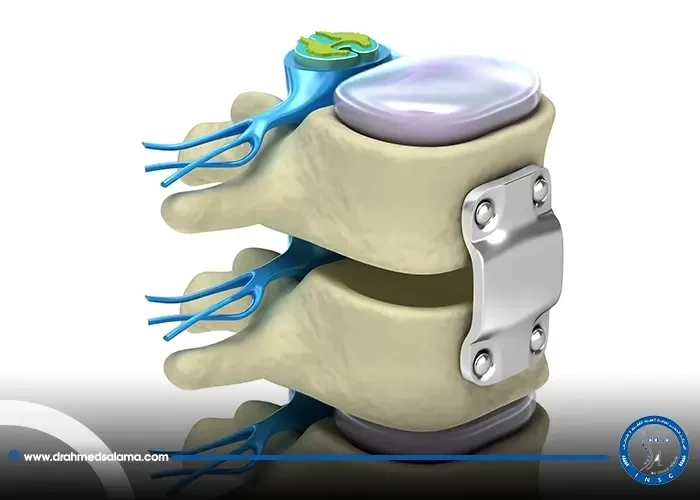
Minimally invasive spine (MIS) surgery is a surgical technique developed to treat spine problems with minimal injury to the muscles and other normal structures in the spine. In general, the goal of MIS surgery is to stabilize the vertebral bones and spinal joints and/or relieve pressure being applied. MIS surgery involves making smaller incisions compared to traditional open surgery, which can lead to reduced pain, blood loss, and a faster recovery time. The surgeon inserts special surgical instruments through these small incisions to access the spine and perform the necessary procedures. The technique has the same surgical outcomes as traditional open spine procedures and is often recommended for selected patients. MIS surgery is an alternative to traditional open surgical procedures for different spinal conditions, including spinal disc protrusions and spinal disc herniation. However, it is important to consult with a spine surgeon to determine if MIS surgery is the best option for an individual's specific condition.
How does MIS surgery differ from traditional open spine surgery?
Minimally invasive spine (MIS) surgery differs from traditional open spine surgery in several ways. The most significant difference is the size of the incision. Traditional open spine surgery requires a large incision, which leads to significant muscle retraction, blood loss, and longer recovery times. In contrast, MIS surgery involves much smaller incisions, allowing for less muscle damage, reduced blood loss, and faster recovery times. During MIS surgery, specialized instruments are used to access the spine through small incisions, while in traditional open surgery, the surgeon must cut through muscle and tissue to reach the affected area. Overall, MIS surgery is less invasive, less traumatic, and leads to a faster return to normal activities. It is important to note that not all spine conditions can be treated with MIS surgery, and some cases may still require traditional open surgery. It is crucial to discuss treatment options with a qualified spine surgeon to determine what type of surgery is best for your specific condition.
What are the potential benefits of MIS surgery?
Minimally invasive spine (MIS) surgery boasts several potential benefits for patients compared to traditional open surgery. One of the primary advantages is less trauma to the body, which can lead to less post-operative pain, less blood loss, and smaller surgical scars. Additionally, MIS surgery can be performed under monitored anesthesia care in an outpatient setting, allowing for a faster recovery time and a quicker return to work and physical activity. Overall, patients undergoing MIS surgery may experience less damage to surrounding tissues, fewer complications, and a higher success rate for treating their spine problems. However, it's important to note that not everyone is a good candidate for MIS surgery, and there are still potential risks and complications to consider. As with any surgical procedure, it's recommended to discuss the potential benefits and drawbacks with a healthcare professional.
How is MIS surgery performed?
Minimally invasive spine surgery (MIS) involves muscle-sparing approaches to the spine using small incisions as access portals. Compared to traditional open spine surgery, MIS surgery is less invasive and requires smaller incisions to access the affected area. MIS surgery is performed using specialized instruments and a monitoring system that allows the surgeon to visualize the affected area in real-time. Endoscope-assisted surgery is commonly performed for the treatment of spinal deformities, herniated discs and infectious spondylitis. Depending on the type of MIS procedure, patients may undergo general anesthesia or receive a local anesthetic with sedation. The surgery is performed through small incisions, typically less than 1 cm in size, and the procedure generally takes 1-3 hours to complete. Patients can expect to experience minimum blood loss and a shorter hospital stay compared to traditional open spine surgery.
What types of spine problems can be treated with MIS surgery?
MIS surgery can be used to treat a variety of spine problems including degenerative disc disease, herniated discs, spinal stenosis, and spinal deformities such as scoliosis. In addition, it can be used for spinal fusion, which is the process of fusing two or more vertebrae together to provide more stability. MIS procedures allow for a smaller incision, which means less tissue damage and a faster recovery time. However, not all spine problems can be treated with MIS surgery, so it's important to consult with a spine specialist to determine the best course of treatment for each individual patient.
Who is a good candidate for MIS surgery?
When it comes to minimally invasive spine (MIS) surgery, not everyone is a good candidate. Generally, patients who are not suitable for traditional open spine surgery are ideal candidates for MIS surgery. Additionally, those who have tried conservative treatments for their neck or lower back pain, but have found no success, may also be good candidates. It's important to keep in mind that a proper patient selection process and guidelines exist to assist MIS surgeons in choosing those who are the right fit for this type of procedure. Ultimately, a doctor will determine if MIS surgery is the best option for an individual based on their specific medical history and condition.
What are the risks and potential complications of MIS surgery?
Despite the numerous benefits of minimally invasive spine surgery (MIS), there are still risks and potential complications associated with this type of procedure. While the risks are similar to those of traditional open spine surgery, MIS may carry a higher risk of certain complications due to the reduced exposure and narrow surgical corridors involved. For example, MIS may increase the risk of nerve damage or spinal fluid leakage. Additionally, patients who have previously undergone spine surgery in the same location or who have pronounced cervical or thoracic deformity may be at a higher risk for complications during MIS. However, it's important to remember that all surgical procedures carry some degree of risk. A qualified surgeon will thoroughly evaluate a patient's health history and individual circumstances to determine whether MIS is the best option for them.
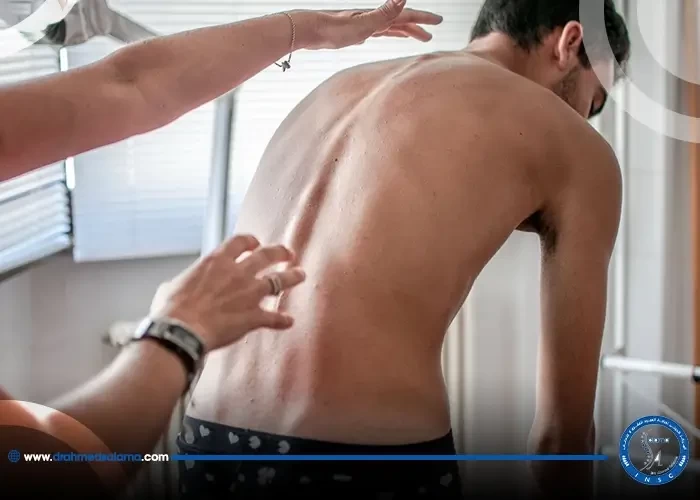
What is the recovery process like after MIS surgery?
After undergoing minimally invasive spine (MIS) surgery, the recovery process is generally quicker and less painful than traditional open spine surgery. Patients are usually able to leave the hospital within a day or two after surgery and return to light activities within a week. However, complete recovery can take anywhere from three to six months, depending on the type of surgery and the patient's individual healing process. During the recovery period, patients may need to avoid certain activities and undergo physical therapy to help strengthen the muscles surrounding the spine. While there are some risks and potential complications associated with MIS surgery, such as infection or nerve damage, these are generally rare. In most cases, patients experience faster recovery times and a reduced reliance on pain medications after MIS surgery compared to open surgery. Overall, the MIS procedure offers many benefits for those seeking relief from spine-related conditions.
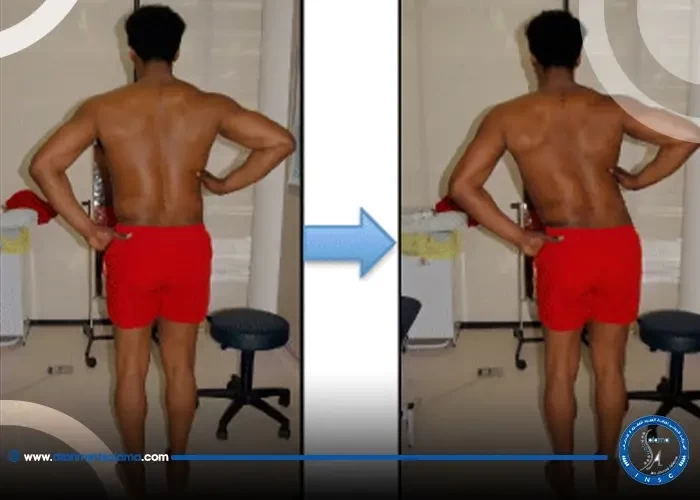
How long does it take to see the results of MIS surgery?
Patients who undergo minimally invasive spine (MIS) surgery can typically expect to see results in the weeks following the procedure. One of the key benefits of MIS surgery is the reduced recovery time compared to traditional open spine surgery, which can take months. However, the specific timeline for seeing results can vary depending on the individual patient and the type of spine problem being treated. In some cases, patients may experience immediate relief from their symptoms, while in others it may take several weeks for the area to heal and for the full benefits of the surgery to be felt. As with any surgical procedure, it is important for patients to follow their doctor's instructions for post-operative care and rehabilitation to ensure the best possible outcome.
What are some alternatives to MIS surgery for spine problems?
While minimally invasive spine (MIS) surgery may be a desirable option for many patients, it is not always the best course of action. Some patients may not be good candidates due to certain health conditions or the nature of their spine problem may require a more invasive approach. Non-surgical alternatives such as physical therapy, chiropractic care, epidural steroid injections, and pain medication may also be effective in managing spine problems. Endoscopic spine surgeries, which use a small tube-like tool to access the spine through a tiny incision, may also be an alternative to MIS surgery for certain conditions. Ultimately, the decision about whether to pursue MIS surgery or an alternative approach will depend on each patient's unique situation and consultation with their medical team.
When will you return to your normal life after a spinal fusion surgery?
The duration of the return to normal life varies from one person to another, but the patient usually begins to gradually return to normal life from the first week after the operation and this continues gradually for up to 6 months after the operation.
How does a spinal fusion patient sleep?
After the procedure, the patient must sleep on his back, keep his back straight, and avoid bending his back.