Nasr City, 52 El Tayaran Street, in front of the Health Insurance Hospital

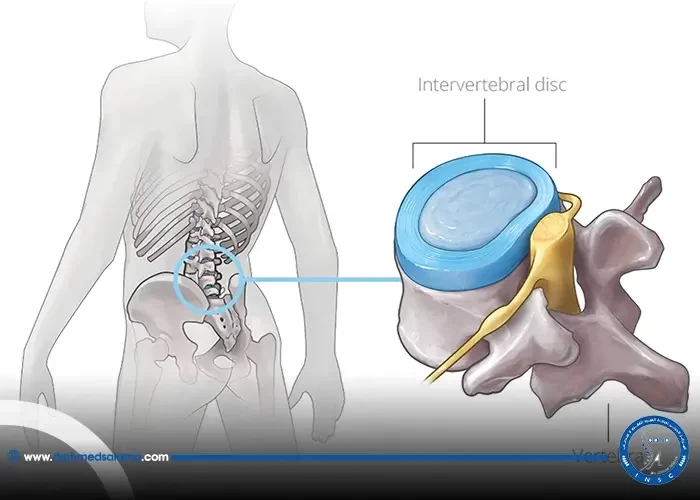
Failed vertebral fixation

In the field of spinal surgeries, vertebral fixation is a common procedure used to stabilize the spine and prevent further damage to the vertebrae. However, despite its popularity, there have been instances where vertebral fixation has failed and resulted in considerable negative outcomes for patients. Today, we will explore the reasons behind the failure of vertebral fixation and how it can be avoided.
Common reasons for failure after spinal fusions
One of the most common reasons for failed spinal fusion is the inability to achieve a solid fusion. This can be due to a variety of factors, including the patient's age, overall health, and lifestyle habits. Other factors that can lead to failed spinal fusion include instrumented fixation and fusion of the thoracic spine, as well as degenerative, traumatic or metastatic instability. Failed back surgery syndrome is characterized by intractable pain and an inability to return to normal activities. In order to prevent failed spinal fusion, it is important for patients to undergo durable reconstruction and follow their surgeon's post-operative guidelines. A nomogram for predicting failure risk in spinal instrumentation can also be used to identify patients who may be at increased risk for complications after spinal surgery. By addressing these common reasons for failure after spinal fusions, patients can increase their chances of a successful outcome and a return to a pain-free life.
Challenges and complications with thoracic spinal fixation
When it comes to spinal fusion surgeries, those involving the thoracic spine present distinct challenges and complications. Pseudarthrosis and junctional kyphosis are commonly observed complications, which make achieving proper fusion and stability difficult. In addition, displacement of screws and hardware failure can lead to further complications and even revision surgeries. While the use of pedicle screws in posterior spinal fixation has shown promising outcomes, it can still lead to complications such as screw loosening or back-out, screw fracture, and improper placement. All these challenges emphasize the importance of choosing durable implant materials and a skilled surgeon. Patients who have undergone spinal fusion surgeries should also closely follow their post-operative rehabilitation plans to optimize the chances of successful bone fusion and avoid complications.
Factors associated with spinal fixation failure
Spinal fixation failure can have various risk factors, which are important to consider before undergoing surgery. Common risk factors include significant spondylolisthesis and grades II to V, along with symptomatic and unremitting pain that has failed conservative treatment. Fixation in osteolytic regions and surgeries near the spinal cord can also increase the likelihood of failure. Moreover, depression and multilevel degenerative disc disease can additionally lead to failed back surgery syndrome. However, advances in posterior fixation with pedicle screws have shown beneficial outcomes in recent years. It is crucial to consider these factors and opt for durable reconstruction to ensure successful spinal fixation. Nomograms can also be used for predicting failure risk in spinal instrumentation. The blog articles highlight the history of spinal fixation materials and implant failure rates while also shedding light on challenges and complications with thoracic spinal fixation, distal junctional failure, and pelvic fixation failure after adult spine surgery.
Importance of durable reconstruction for patients
When it comes to spinal fusion surgery, failure can occur for a variety of reasons. One key factor in preventing failure is ensuring durable reconstruction for patients. This means using biomaterials and spinal implants that can withstand the stress and demands placed on them. Additionally, non-fusion palliative spine surgery without reconstruction may be safe and effective for some patients with spinal metastasis. The use of cages, for example, has become increasingly prevalent in spine surgery as they provide added stability and support to the affected area. While failed fusion in the cervical spine may have multifactorial causes, ensuring durable reconstruction for patients can help prevent complications and improve outcomes.
Nomogram for predicting failure risk in spinal instrumentation
The previous sections of this blog have discussed the challenges and complications associated with spinal fixation, as well as the factors and reasons for failure after spinal fusions. However, there is now a novel nomogram available for predicting the failure risk in spinal instrumentation. This nomogram includes gender, age, presence or absence of scoliosis, and unilateral or bilateral fixation. By utilizing this tool, medical professionals can better assess the risk of screw loosening and other complications associated with spinal fixation. This information can help them tailor the surgical plan to ensure a more durable reconstruction and better outcomes for their patients. By incorporating this nomogram into their practice, physicians can better anticipate the likelihood of failure and make more informed decisions in spinal instrumentation surgeries.
Distal junctional failure: two case reports
Distal junctional failure is a rare but serious complication that can occur after spinal fusions. As discussed in the previous sections, there are several factors that can contribute to this type of failure, including instrumentation failure, surgical technique, and patient-related factors. Two case reports of distal junctional failure following instrumented fusion of the lumbar spine, which were presented in this section, highlight the importance of careful patient selection and surgical planning. In both cases, the patients experienced worsening neurology due to nontraumatic fracture of a lower vertebral level, which resulted in DJF. It is crucial for surgeons to be aware of this potential complication and take steps to minimize the risk, such as using supplemental fixation techniques and careful selection of fusion levels. By doing so, patients can have a better chance of achieving a durable reconstruction that will alleviate their back pain and improve their quality of life.
Pelvic fixation failure after adult spine surgery
Pelvic fixation remains a challenging aspect of spinal deformity surgery, and revision surgery due to acute pelvic instrumentation failure within 6 months of primary surgery has been reported in some cases. As seen in previous sections of the blog, failure of spinal fusion can result from numerous factors, including challenges and complications associated with thoracic spinal fixation, non-union at the L5/S1 level, and distal junctional failure. In addition, there are risks associated with long segment fusions in patients with adult spinal deformity, including proximal junctional failure (PJF) and failure of pelvic screws.
However, despite the potential risks, pelvic fixation is still a widely accepted technique in adult spinal deformity surgery, with the goal of restoring the optimal sagittal balance for patients. It is essential to consider factors associated with spinal fixation failure, such as patient demographics, surgical correction magnitude, and failure mechanisms. In addition, new predictive tools, such as a nomogram, can assist in determining the risk of failure in spinal instrumentation.
For patients who experience pelvic fixation failure or PJF after long segment fusions in ASD correction, surgical treatment is crucial. Therefore, it is essential to reconstruct spinal deformities durably with appropriate materials and techniques to minimize the risk of failure. Finally, the history of spinal fixation materials and implant failure rates demonstrates the importance of constantly evolving techniques and materials to minimize the risks associated with adult spinal deformity surgeries.
History of spinal fixation materials and implant failure rates
When discussing the failure of vertebral fixation in spinal surgery, it's essential to understand the history of spinal fixation materials and implant failure rates. Over the last decade, pedicle fixation systems have evolved, and modifications in spinal fusion techniques have been developed to increase fusion rates and reduce implant failure rates. However, many challenges and complications come with thoracic spinal fixation, and factors such as patient age, sex, smoking, and preexisting medical conditions can increase the risk of spinal fixation failure. It's imperative to provide patients with durable reconstruction to minimize the risk of failure and preserve spinal function. Additionally, utilizing a nomogram to predict failure risk and analyzing data on failed internal fixation can help improve future surgical outcomes. Overall, while there have been significant advancements in spinal fixation materials, it's crucial to continue learning from past failures to ensure successful outcomes in spinal surgery.
Advantages of posterior fixation with pedicle screws
One of the most effective techniques for spinal fixation is posterior fixation using pedicle screws. This technique offers numerous advantages, such as superior correction of spinal deformities and reduced rates of loss of fixation compared to other techniques. Furthermore, incorporating fewer motion segments than long-segment pedicle fixation provides a main advantage. However, despite the benefits, spinal fixation failure can still occur due to various factors, including vertebral body fractures and instrumentation failures. It is essential to ensure durable reconstruction for patients to avoid such complications. Nomograms can be used to predict failure risk in spinal instrumentation, while case studies can highlight the importance of addressing distal junctional and pelvic fixation failures. By understanding the history of spinal fixation materials and acknowledging the potential challenges, spinal fusion failure can be prevented, ultimately reducing back pain and improving the quality of life for those who undergo these procedures.
Reasons for spinal fusion failure in alleviating back pain
Despite advancements in spinal fusion surgery, there are still instances where it fails to provide long-term relief from back pain. As discussed in previous sections, common reasons for such failures can include inadequate fusion, altered biomechanics, and changes in load distribution. However, there are other factors that contribute to the failure of spinal fusion surgery. Implant failure or loosening, infection, and pseudoarthrosis are some complications that can occur post-surgery, leading to persistent pain. Surgeons also believe that spinal laminectomy, a procedure to treat spinal stenosis, is performed too frequently and can negatively impact the overall outcome of surgery. Chronic post-surgical spinal pain, also known as failed back or failed fusion syndrome, can be a result of any of the above factors, making durable reconstruction and proper postoperative care crucial for successful outcomes in spinal fusion surgery.
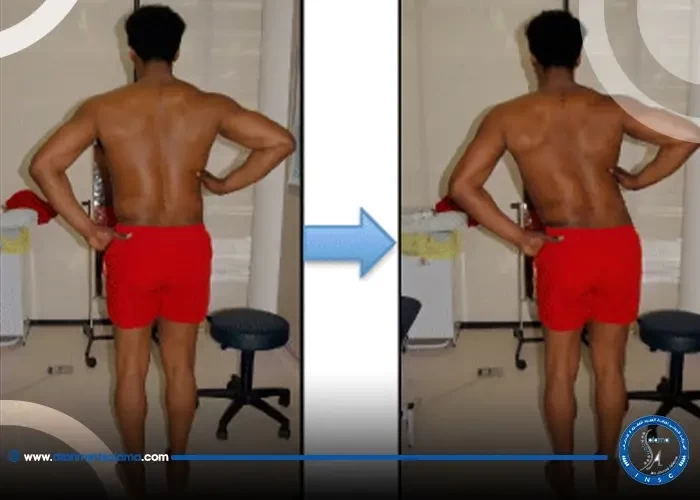
How do I know if the vertebral fusion procedure failed?
You may experience some symptoms after the procedure, indicating a failure of the spinal fusion procedure. These symptoms include severe wound infections, severe pain that does not go away with medication and painkillers, and discomfort from pre-operative pain.
When will you return to your normal life after a spinal fusion surgery?
The pain may disappear within a week of the spinal fusion procedure, and the patient will gradually begin to improve until he returns to his normal life 6 months after the procedure.